Postnatal test can be done by using both newborn and maternal blood sample.
As antibodies had not fully develops in newborn, only the ABO forward grouping is done on newborn sample. Rh typing is done in order to identify the baby’s Rh group. Weak D test is also performed if the baby is Rh negative. Positive Rh result obtain is not solely indicates that the newborn is Rh-positive, but it may also indicate the presence of maternal antibody that heavily coated on newborn’s RBC. Furthermore, newborns who were transfused while intrauterine often type Rh negative or weakly Rh positive. Therefore, it is impossible to get a proper Rh type without heating fetal RBC first to eluate off the antibody. ABO and Rh typing for maternal sample is done similarly to prenatal test.
- Direct antiglobulin test (DAT) and elution.
DAT test should be performs on cord blood RBCs in identifying in vivo sensitization by maternal antibody. There are varies factors that contribute to the strength of DAT, which include maternal antibody strength, number of antigenic site directed by maternal antibody and total amount of blood infant receive from transfusion. Elution is done when the DAT outcome is positive. In addition, elution is also performed if the baby is symptomatic even if the DAT test shows negative result. It is unnecessary to perform elution on infant’s RBC if there is available of maternal blood and a single antibody is identified. If however, the maternal serum is negative for unexpected antibodies, so it is suggested of having ABO antibodies or an antibody to a low-frequency antigen. Diagnosing a low-frequency antigen can be aids by testing the eluate with paternal RBCs. Even though the antibody screening tests and panels give negative result, testing the maternal serum against paternal serum confirms the presence of antibody. As stated above, elution is done after getting the result of DAT. Type of cells used to test eluate depends on antibody found on mother. Below are 2 examples of situations that shows usage of different types of elute cells.
· Mom: anti-A, anti-B and/or anti-AB; negative antibody screening
Baby: A or B blood group
o Test eluate against screening cells, A1 and B cells.
o May performed Lui freeze-thaw or acid elution.
o Strength of DAT varies depends on maternal antibody strength, no of antigenic sites for antigen to which maternal antibody is directed, how much blood the infants has received from transfusion.
· Mom: positive antibody screen
o Perform acid elution.
o Against the same cells that react in mother ab identification panel.
o Include reagent A1 and B cells if mother is group O, baby is A or B.
- Antibody screening and identification
Antibody screening only performed on maternal sample, as the newborn did not fully develop their own antibodies. It is done similar to those procedure perform for prenatal test.
- Fetal-maternal hemorrhage (FMH).
Protection of mother against the immunizing effects of Rh-positive fetal RBCs is vital, therefore it is important for the Rh-negative women to receive appropriate amount of RhIG. The half-life of the RhIG in the absence of significant mixing of fetal with maternal circulation, called fetal-maternal hemorrhage, is approximately 21 days. Two tests are commonly used to detect and quantify FMH: Rosette test and Kleihauer-Betke test.
i. Rosette test
o Qualitative test.
o Used to detect FMH greater than 30mL.
o Procedure:
I. Incubate suspension of maternal blood with anti-D
II. Fetal Rh-positive RBCs in maternal blood react with anti-D.
III. Wash unbound antibody.
IV. Add suspension of group O, Rh-positive cells.
V. Reaction between anti-D with both O Rh-positive and fetal Rh-
positive RBCs, form agglutination in a rosette form.
VI. Examine the suspension microscopically.
o Presence of a certain number of clumps in a defined number of microscopic fields indicates positive result.
o Less than 30mL indicates negative result.
o Quantitative test must be performed to estimate the number of vials of RhIg needed.
ii. Kleihauer-Betke (KB) test.
o Quantitative test.
o Must be performed if positive rosette test.
o Done to estimate the needed number of RhIG vials.
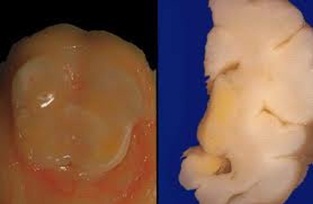
o Principle is based on the resistance of fetal hemoglobin to acid elution.
o The percentage of fetal cells in maternal sample can be used to calculate the volume of FMH and the appropriate number of vials of RhIG.
o Indication:
- Determine possible FMH in the newborn.
- Aid in diagnosis of certain types of anemia in adults
- Assess the magnitude of FMH
o Calculate dosage of RhIg to be given through the percentage of fetal cells in maternal sample.
iii. Flow cytometry
o Similar purpose with KB test.
o Less available compare to KB test.
o Done by analyzing mixture of maternal sample, anti-D and fluorescein-labeled IgG by fluorescein-activated cell sorter.